Looking At Pes Planus
Overview

In a normal foot, the tendons in your foot and lower leg work together to form the arch. When the tendons all pull properly, your foot forms a moderate, normal arch. When the tendons do not pull together properly, there is little or no arch, called flat foot or fallen arch. Children are born with flat feet. In infants and toddlers, prior to walking, the longitudinal arch is not developed and flat feet are normal. As children begin standing on their toes, the muscles start to develop and an arch appears. The arch continues to develop throughout childhood, and by adulthood most people have developed normal arches. But in some cases the arch doesn?t form completely.
Causes
You can have a tendency towards fallen arches from birth. Up through the toddler stage, it is common to have flat feet. Throughout childhood, arches tend to normally develop. For reasons not well understood, however, in some cases the feet stay flat and the arch never forms. In many cases this abnormality does not cause symptoms or require any treatment. In other cases, it is due to a condition called tarsal coalition. This occurs when some of the foot bones fuse.
Symptoms
Fallen arches may induce pain in the heel, the inside of the arch, the ankle, and may even extend up the body into the leg (shin splints), knee, lower back and hip. You may also experience inflammation (swelling, redness, heat and pain) along the inside of the ankle (along the posterior tibial tendon). Additionally, you may notice some changes in the way your foot looks. Your ankle may begin to turn inward (pronate), causing the bottom of your heel to tilt outward. Other secondary symptoms may also show up as the condition progresses, such as hammertoes or bunions. You may also want to check your footprint after you step out of the shower. (It helps if you pretend you?re in a mystery novel, and you?re leaving wet, footprinty clues that will help crack the case.) Normally, you can see a clear imprint of the front of your foot (the ball and the toes) the heel, and the outside edge of your foot. There should be a gap (i.e. no footprinting) along the inside where your arches are. If your foot is flat, it?ll probably leave an imprint of the full bottom of your foot-no gap to be had. Your shoes may also be affected: because the ankle tilts somewhat with this condition, the heel of your shoes may become more worn on one side than another.
Diagnosis
Most children and adults with flatfeet do not need to see a physician for diagnosis or treatment. However, it is a good idea to see a doctor if the feet tire easily or are painful after standing, it is difficult to move the foot around or stand on the toes, the foot aches, especially in the heel or arch, and there is swelling on the inner side of the foot, the pain interferes with activity or the person has been diagnosed with rheumatoid arthritis. Most flatfeet are diagnosed during physical examination. During the exam, the foot may be wetted and the patient asked to stand on a piece of paper. An outline of the entire foot will indicate a flattened arch. Also, when looking at the feet from behind, the ankle and heel may appear to lean inward (pronation). The patient may be asked to walk so the doctor can see how much the arch flattens during walking. The doctor may also examine the patient's shoes for signs of uneven wear, ask questions about a family history of flatfeet, and inquire about known neurological or muscular diseases. Imaging tests may be used to help in the diagnosis. If there is pain or the arch does not appear when the foot is flexed, x-rays are taken to determine the cause. If tarsal coalition is suspected, computed tomography (CT scan) may be performed, and if an injury to the tendons is suspected, magnetic resonance imaging (MRI scan) may be performed.
Can you fix a fallen arch?
Non Surgical Treatment
Custom orthotics are specially designed insoles, which are made for your by prescription. This is done by taking a plaster cast of the foot in its neutral position and is then sent to a laboratory, with your prescription to be made to your exact specifications. The insole then correctly aligns your foot and as a result your body. This will relieve abnormal strain of tissues and structures which can cause pain. For less severe mal-alignments or for sports use a wide variety of temporary insoles.
Surgical Treatment

A better approach is to strengthen the weakened ligaments with Prolotherapy, supplemented by an arch support if the condition has existed for several years. Chronic pain is most commonly due to tendon and ligament weakness, or cartilage deterioration. The safest and most effective natural medicine treatment for repairing tendon, ligament and cartilage damage is Prolotherapy. In simple terms, Prolotherapy stimulates the body to repair painful areas. It does so by inducing a mild inflammatory reaction in the weakened ligaments and cartilage. Since the body heals by inflammation, Prolotherapy stimulates healing. Prolotherapy offers the most curative results in treating chronic pain. It effectively eliminates pain because it attacks the source: the fibro-osseous junction, an area rich in sensory nerves. What?s more, the tissue strengthening and pain relief stimulated by Prolotherapy is permanent.
Prevention
Going barefoot, particularly over terrain such as a beach where muscles are given a good workout, is good for all but the most extremely flatfooted, or those with certain related conditions such as plantar fasciitis. Ligament laxity is also among the factors known to be associated with flat feet. One medical study in India with a large sample size of children who had grown up wearing shoes and others going barefoot found that the longitudinal arches of the bare footers were generally strongest and highest as a group, and that flat feet were less common in children who had grown up wearing sandals or slippers than among those who had worn closed-toe shoes. Focusing on the influence of footwear on the prevalence of pes planus, the cross-sectional study performed on children noted that wearing shoes throughout early childhood can be detrimental to the development of a normal or a high medial longitudinal arch. The vulnerability for flat foot among shoe-wearing children increases if the child has an associated ligament laxity condition. The results of the study suggest that children be encouraged to play barefooted on various surfaces of terrain and that slippers and sandals are less harmful compared to closed-toe shoes. It appeared that closed-toe shoes greatly inhibited the development of the arch of the foot more so than slippers or sandals. This conclusion may be a result of the notion that intrinsic muscle activity of the arch is required to prevent slippers and sandals from falling off the child?s foot.
After Care
Time off work depends on the type of work as well as the surgical procedures performed. . A patient will be required to be non-weight bearing in a cast or splint and use crutches for four to twelve weeks. Usually a patient can return to work in one to two weeks if they are able to work while seated. If a person's job requires standing and walking, return to work may take several weeks. Complete recovery may take six months to a full year. Complications can occur as with all surgeries, but are minimized by strictly following your surgeon's post-operative instructions. The main complications include infection, bone that is slow to heal or does not heal, progression or reoccurrence of deformity, a stiff foot, and the need for further surgery. Many of the above complications can be avoided by only putting weight on the operative foot when allowed by your surgeon.

In a normal foot, the tendons in your foot and lower leg work together to form the arch. When the tendons all pull properly, your foot forms a moderate, normal arch. When the tendons do not pull together properly, there is little or no arch, called flat foot or fallen arch. Children are born with flat feet. In infants and toddlers, prior to walking, the longitudinal arch is not developed and flat feet are normal. As children begin standing on their toes, the muscles start to develop and an arch appears. The arch continues to develop throughout childhood, and by adulthood most people have developed normal arches. But in some cases the arch doesn?t form completely.
Causes
You can have a tendency towards fallen arches from birth. Up through the toddler stage, it is common to have flat feet. Throughout childhood, arches tend to normally develop. For reasons not well understood, however, in some cases the feet stay flat and the arch never forms. In many cases this abnormality does not cause symptoms or require any treatment. In other cases, it is due to a condition called tarsal coalition. This occurs when some of the foot bones fuse.
Symptoms
Fallen arches may induce pain in the heel, the inside of the arch, the ankle, and may even extend up the body into the leg (shin splints), knee, lower back and hip. You may also experience inflammation (swelling, redness, heat and pain) along the inside of the ankle (along the posterior tibial tendon). Additionally, you may notice some changes in the way your foot looks. Your ankle may begin to turn inward (pronate), causing the bottom of your heel to tilt outward. Other secondary symptoms may also show up as the condition progresses, such as hammertoes or bunions. You may also want to check your footprint after you step out of the shower. (It helps if you pretend you?re in a mystery novel, and you?re leaving wet, footprinty clues that will help crack the case.) Normally, you can see a clear imprint of the front of your foot (the ball and the toes) the heel, and the outside edge of your foot. There should be a gap (i.e. no footprinting) along the inside where your arches are. If your foot is flat, it?ll probably leave an imprint of the full bottom of your foot-no gap to be had. Your shoes may also be affected: because the ankle tilts somewhat with this condition, the heel of your shoes may become more worn on one side than another.
Diagnosis
Most children and adults with flatfeet do not need to see a physician for diagnosis or treatment. However, it is a good idea to see a doctor if the feet tire easily or are painful after standing, it is difficult to move the foot around or stand on the toes, the foot aches, especially in the heel or arch, and there is swelling on the inner side of the foot, the pain interferes with activity or the person has been diagnosed with rheumatoid arthritis. Most flatfeet are diagnosed during physical examination. During the exam, the foot may be wetted and the patient asked to stand on a piece of paper. An outline of the entire foot will indicate a flattened arch. Also, when looking at the feet from behind, the ankle and heel may appear to lean inward (pronation). The patient may be asked to walk so the doctor can see how much the arch flattens during walking. The doctor may also examine the patient's shoes for signs of uneven wear, ask questions about a family history of flatfeet, and inquire about known neurological or muscular diseases. Imaging tests may be used to help in the diagnosis. If there is pain or the arch does not appear when the foot is flexed, x-rays are taken to determine the cause. If tarsal coalition is suspected, computed tomography (CT scan) may be performed, and if an injury to the tendons is suspected, magnetic resonance imaging (MRI scan) may be performed.
Can you fix a fallen arch?
Non Surgical Treatment
Custom orthotics are specially designed insoles, which are made for your by prescription. This is done by taking a plaster cast of the foot in its neutral position and is then sent to a laboratory, with your prescription to be made to your exact specifications. The insole then correctly aligns your foot and as a result your body. This will relieve abnormal strain of tissues and structures which can cause pain. For less severe mal-alignments or for sports use a wide variety of temporary insoles.
Surgical Treatment

A better approach is to strengthen the weakened ligaments with Prolotherapy, supplemented by an arch support if the condition has existed for several years. Chronic pain is most commonly due to tendon and ligament weakness, or cartilage deterioration. The safest and most effective natural medicine treatment for repairing tendon, ligament and cartilage damage is Prolotherapy. In simple terms, Prolotherapy stimulates the body to repair painful areas. It does so by inducing a mild inflammatory reaction in the weakened ligaments and cartilage. Since the body heals by inflammation, Prolotherapy stimulates healing. Prolotherapy offers the most curative results in treating chronic pain. It effectively eliminates pain because it attacks the source: the fibro-osseous junction, an area rich in sensory nerves. What?s more, the tissue strengthening and pain relief stimulated by Prolotherapy is permanent.
Prevention
Going barefoot, particularly over terrain such as a beach where muscles are given a good workout, is good for all but the most extremely flatfooted, or those with certain related conditions such as plantar fasciitis. Ligament laxity is also among the factors known to be associated with flat feet. One medical study in India with a large sample size of children who had grown up wearing shoes and others going barefoot found that the longitudinal arches of the bare footers were generally strongest and highest as a group, and that flat feet were less common in children who had grown up wearing sandals or slippers than among those who had worn closed-toe shoes. Focusing on the influence of footwear on the prevalence of pes planus, the cross-sectional study performed on children noted that wearing shoes throughout early childhood can be detrimental to the development of a normal or a high medial longitudinal arch. The vulnerability for flat foot among shoe-wearing children increases if the child has an associated ligament laxity condition. The results of the study suggest that children be encouraged to play barefooted on various surfaces of terrain and that slippers and sandals are less harmful compared to closed-toe shoes. It appeared that closed-toe shoes greatly inhibited the development of the arch of the foot more so than slippers or sandals. This conclusion may be a result of the notion that intrinsic muscle activity of the arch is required to prevent slippers and sandals from falling off the child?s foot.
After Care
Time off work depends on the type of work as well as the surgical procedures performed. . A patient will be required to be non-weight bearing in a cast or splint and use crutches for four to twelve weeks. Usually a patient can return to work in one to two weeks if they are able to work while seated. If a person's job requires standing and walking, return to work may take several weeks. Complete recovery may take six months to a full year. Complications can occur as with all surgeries, but are minimized by strictly following your surgeon's post-operative instructions. The main complications include infection, bone that is slow to heal or does not heal, progression or reoccurrence of deformity, a stiff foot, and the need for further surgery. Many of the above complications can be avoided by only putting weight on the operative foot when allowed by your surgeon.
Heel Discomfort The Causes, Warning Signs And Cure Choices
Overview

Heel pain is a very common foot problem. The sufferer usually feels pain either under the heel (planter fasciitis) or just behind it (Achilles tendinitis), where the Achilles tendon connects to the heel bone. Even though heel pain can be severe and sometimes disabling, it is rarely a health threat. Heel pain is typically mild and usually disappears on its own; however, in some cases the pain may persist and become chronic (long-term).
Causes
The most common local causes of heel pain include. Plantar fasciitis, plantar fasciitis is a painful inflammation of the plantar fascia, a fibrous band of tissue on the sole of the foot that helps to support the arch. Plantar fasciitis occurs when the plantar fascia is overloaded or overstretched. This causes small tears in the fibers of the fascia, especially where the fascia meets the heel bone. Plantar fasciitis may develop in just about anyone but it is particularly common in the following groups of people: people with diabetes, obese people, pregnant women, runners, volleyball players, tennis players and people who participate in step aerobics or stair climbing. You also can trigger plantar fasciitis by pushing a large appliance or piece of furniture or by wearing worn out or poorly constructed shoes. In athletes, plantar fasciitis may follow a period of intense training, especially in runners who push themselves to run longer distances. People with flat feet have a higher risk of developing plantar fasciitis. Heel spur, a heel spur is an abnormal growth of bone at the area where the plantar fascia attaches to the heel bone. It is caused by long-term strain on the plantar fascia and muscles of the foot, especially in obese people, runners or joggers. As in plantar fasciitis, shoes that are worn out, poorly fitting or poorly constructed can aggravate the problem. Heel spurs may not be the cause of heel pain even when seen on an X-ray. In fact, they may develop as a reaction to plantar fasciitis. Calcaneal apophysitis, in this condition, the center of the heel bone becomes irritated as a result of a new shoe or increased athletic activity. This pain occurs in the back of the heel, not the bottom. Calcaneal apophysitis is a fairly common cause of heel pain in active, growing children between the ages of 8 and 14. Although almost any boy or girl can be affected, children who participate in sports that require a lot of jumping have the highest risk of developing this condition. Bursitis means inflammation of a bursa, a sac that lines many joints and allows tendons and muscles to move easily when the joint is moving. In the heel, bursitis may cause pain at the underside or back of the heel. In some cases, heel bursitis is related to structural problems of the foot that cause an abnormal gait (way of walking). In other cases, wearing shoes with poorly cushioned heels can trigger bursitis. Pump bump, this condition, medically known as posterior calcaneal exostosis, is an abnormal bony growth at the back of the heel. It is especially common in young women, in whom it is often related to long-term bursitis caused by pressure from pump shoes. Like other parts of the foot, the heel can be bumped and bruised accidentally. Typically, this happens as a "stone bruise," an impact injury caused by stepping on a sharp object while walking barefoot. In most cases, Achilles tendonitis (inflammation of the Achilles tendon) is triggered by overuse, especially by excessive jumping during sports. However, it also can be related to poorly fitting shoes if the upper back portion of a shoe digs into the Achilles tendon at the back of the heel. Less often, it is caused by an inflammatory illness, such as ankylosing spondylitis (also called axial spondylarthritis), reactive arthritis, gout or rheumatoid arthritis. Compression of a small nerve (a branch of the lateral plantar nerve) can cause pain, numbness or tingling in the heel area. In many cases, this nerve compression is related to a sprain, fracture or varicose (swollen) vein near the heel.
Symptoms
The primary symptom is pain in the heel area that varies in severity and location. The pain is commonly intense when getting out of bed or a chair. The pain often lessens when walking.
Diagnosis
Your doctor will perform a physical exam and ask questions about your medical history and symptoms, such as have you had this type of heel pain before? When did your pain begin? Do you have pain upon your first steps in the morning or after your first steps after rest? Is the pain dull and aching or sharp and stabbing? Is it worse after exercise? Is it worse when standing? Did you fall or twist your ankle recently? Are you a runner? If so, how far and how often do you run? Do you walk or stand for long periods of time? What kind of shoes do you wear? Do you have any other symptoms? Your doctor may order a foot x-ray. You may need to see a physical therapist to learn exercises to stretch and strengthen your foot. Your doctor may recommend a night splint to help stretch your foot. Surgery may be recommended in some cases.
Non Surgical Treatment
Anti-inflammatory medication. Heel stretching exercise. Ice application to painful area - twice a day or more, for 10 - 15 minutes. Rest. Supportive, well-fitting, padded shoes. Heel cup, felt pads or orthotics. Night splints - stretches injured fascia and allows healing. Basic treatment. First thing in the morning, before getting out of bed -- massage the bottom of the affected foot or feet for at least five minutes. Ensure that the plantar is stretched and warmed up so that overnight healing remains intact. Before stepping out of bed, be sure that you have soft, padded, supportive shoes or slippers to wear, especially if your flooring is hard, tile or uncarpeted flooring.
Surgical Treatment
Extracorporeal shockwave therapy (EST) is a fairly new type of non-invasive treatment. Non-invasive means it does not involve making cuts into your body. EST involves using a device to deliver high-energy soundwaves into your heel. The soundwaves can sometimes cause pain, so a local anaesthetic may be used to numb your heel. It is claimed that EST works in two ways. It is thought to have a "numbing" effect on the nerves that transmit pain signals to your brain, help stimulate and speed up the healing process. However, these claims have not yet been definitively proven. The National Institute for Health and Care Excellence (NICE) has issued guidance about the use of EST for treating plantar fasciitis. NICE states there are no concerns over the safety of EST, but there are uncertainties about how effective the procedure is for treating heel pain. Some studies have reported that EST is more effective than surgery and other non-surgical treatments, while other studies found the procedure to be no better than a placebo (sham treatment).
deelsonheels
Prevention

You should always wear footwear that is appropriate for your environment and day-to-day activities. Wearing high heels when you go out in the evening is unlikely to be harmful. However, wearing them all week at work may damage your feet, particularly if your job involves a lot of walking or standing. Ideally, you should wear shoes with laces and a low to moderate heel that supports and cushions your arches and heels. Avoid wearing shoes with no heels. Do not walk barefoot on hard ground, particularly while on holiday. Many cases of heel pain occur when a person protects their feet for 50 weeks of the year and then suddenly walks barefoot while on holiday. Their feet are not accustomed to the extra pressure, which causes heel pain. If you do a physical activity, such as running or another form of exercise that places additional strain on your feet, you should replace your sports shoes regularly. Most experts recommend that sports shoes should be replaced after you have done about 500 miles in them. It is also a good idea to always stretch after exercising, and to make strength and flexibility training a part of your regular exercise routine.

Heel pain is a very common foot problem. The sufferer usually feels pain either under the heel (planter fasciitis) or just behind it (Achilles tendinitis), where the Achilles tendon connects to the heel bone. Even though heel pain can be severe and sometimes disabling, it is rarely a health threat. Heel pain is typically mild and usually disappears on its own; however, in some cases the pain may persist and become chronic (long-term).
Causes
The most common local causes of heel pain include. Plantar fasciitis, plantar fasciitis is a painful inflammation of the plantar fascia, a fibrous band of tissue on the sole of the foot that helps to support the arch. Plantar fasciitis occurs when the plantar fascia is overloaded or overstretched. This causes small tears in the fibers of the fascia, especially where the fascia meets the heel bone. Plantar fasciitis may develop in just about anyone but it is particularly common in the following groups of people: people with diabetes, obese people, pregnant women, runners, volleyball players, tennis players and people who participate in step aerobics or stair climbing. You also can trigger plantar fasciitis by pushing a large appliance or piece of furniture or by wearing worn out or poorly constructed shoes. In athletes, plantar fasciitis may follow a period of intense training, especially in runners who push themselves to run longer distances. People with flat feet have a higher risk of developing plantar fasciitis. Heel spur, a heel spur is an abnormal growth of bone at the area where the plantar fascia attaches to the heel bone. It is caused by long-term strain on the plantar fascia and muscles of the foot, especially in obese people, runners or joggers. As in plantar fasciitis, shoes that are worn out, poorly fitting or poorly constructed can aggravate the problem. Heel spurs may not be the cause of heel pain even when seen on an X-ray. In fact, they may develop as a reaction to plantar fasciitis. Calcaneal apophysitis, in this condition, the center of the heel bone becomes irritated as a result of a new shoe or increased athletic activity. This pain occurs in the back of the heel, not the bottom. Calcaneal apophysitis is a fairly common cause of heel pain in active, growing children between the ages of 8 and 14. Although almost any boy or girl can be affected, children who participate in sports that require a lot of jumping have the highest risk of developing this condition. Bursitis means inflammation of a bursa, a sac that lines many joints and allows tendons and muscles to move easily when the joint is moving. In the heel, bursitis may cause pain at the underside or back of the heel. In some cases, heel bursitis is related to structural problems of the foot that cause an abnormal gait (way of walking). In other cases, wearing shoes with poorly cushioned heels can trigger bursitis. Pump bump, this condition, medically known as posterior calcaneal exostosis, is an abnormal bony growth at the back of the heel. It is especially common in young women, in whom it is often related to long-term bursitis caused by pressure from pump shoes. Like other parts of the foot, the heel can be bumped and bruised accidentally. Typically, this happens as a "stone bruise," an impact injury caused by stepping on a sharp object while walking barefoot. In most cases, Achilles tendonitis (inflammation of the Achilles tendon) is triggered by overuse, especially by excessive jumping during sports. However, it also can be related to poorly fitting shoes if the upper back portion of a shoe digs into the Achilles tendon at the back of the heel. Less often, it is caused by an inflammatory illness, such as ankylosing spondylitis (also called axial spondylarthritis), reactive arthritis, gout or rheumatoid arthritis. Compression of a small nerve (a branch of the lateral plantar nerve) can cause pain, numbness or tingling in the heel area. In many cases, this nerve compression is related to a sprain, fracture or varicose (swollen) vein near the heel.
Symptoms
The primary symptom is pain in the heel area that varies in severity and location. The pain is commonly intense when getting out of bed or a chair. The pain often lessens when walking.
Diagnosis
Your doctor will perform a physical exam and ask questions about your medical history and symptoms, such as have you had this type of heel pain before? When did your pain begin? Do you have pain upon your first steps in the morning or after your first steps after rest? Is the pain dull and aching or sharp and stabbing? Is it worse after exercise? Is it worse when standing? Did you fall or twist your ankle recently? Are you a runner? If so, how far and how often do you run? Do you walk or stand for long periods of time? What kind of shoes do you wear? Do you have any other symptoms? Your doctor may order a foot x-ray. You may need to see a physical therapist to learn exercises to stretch and strengthen your foot. Your doctor may recommend a night splint to help stretch your foot. Surgery may be recommended in some cases.
Non Surgical Treatment
Anti-inflammatory medication. Heel stretching exercise. Ice application to painful area - twice a day or more, for 10 - 15 minutes. Rest. Supportive, well-fitting, padded shoes. Heel cup, felt pads or orthotics. Night splints - stretches injured fascia and allows healing. Basic treatment. First thing in the morning, before getting out of bed -- massage the bottom of the affected foot or feet for at least five minutes. Ensure that the plantar is stretched and warmed up so that overnight healing remains intact. Before stepping out of bed, be sure that you have soft, padded, supportive shoes or slippers to wear, especially if your flooring is hard, tile or uncarpeted flooring.
Surgical Treatment
Extracorporeal shockwave therapy (EST) is a fairly new type of non-invasive treatment. Non-invasive means it does not involve making cuts into your body. EST involves using a device to deliver high-energy soundwaves into your heel. The soundwaves can sometimes cause pain, so a local anaesthetic may be used to numb your heel. It is claimed that EST works in two ways. It is thought to have a "numbing" effect on the nerves that transmit pain signals to your brain, help stimulate and speed up the healing process. However, these claims have not yet been definitively proven. The National Institute for Health and Care Excellence (NICE) has issued guidance about the use of EST for treating plantar fasciitis. NICE states there are no concerns over the safety of EST, but there are uncertainties about how effective the procedure is for treating heel pain. Some studies have reported that EST is more effective than surgery and other non-surgical treatments, while other studies found the procedure to be no better than a placebo (sham treatment).
deelsonheels
Prevention

You should always wear footwear that is appropriate for your environment and day-to-day activities. Wearing high heels when you go out in the evening is unlikely to be harmful. However, wearing them all week at work may damage your feet, particularly if your job involves a lot of walking or standing. Ideally, you should wear shoes with laces and a low to moderate heel that supports and cushions your arches and heels. Avoid wearing shoes with no heels. Do not walk barefoot on hard ground, particularly while on holiday. Many cases of heel pain occur when a person protects their feet for 50 weeks of the year and then suddenly walks barefoot while on holiday. Their feet are not accustomed to the extra pressure, which causes heel pain. If you do a physical activity, such as running or another form of exercise that places additional strain on your feet, you should replace your sports shoes regularly. Most experts recommend that sports shoes should be replaced after you have done about 500 miles in them. It is also a good idea to always stretch after exercising, and to make strength and flexibility training a part of your regular exercise routine.
Leg Length Discrepancy And Medical Procedures
Overview
Surgery is another option. In some cases the longer extremity can be shortened, but a major shortening may weaken the muscles of the extremity. In growing children, lower extremities can also be equalized by a surgical procedure that stops the growth at one or two sites of the longer extremity, while leaving the remaining growth undisturbed. Your physician can tell you how much equalization can be attained by surgically halting one or more growth centers. The procedure is performed under X-ray control through very small incisions in the knee area. This procedure will not cause an immediate correction in length. Instead, the LLD will gradually decrease as the opposite extremity continues to grow and "catch up." Timing of the procedure is critical; the goal is to attain equal length of the extremities at skeletal maturity, usually in the mid- to late teens. Disadvantages of this option include the possibility of slight over-correction or under-correction of the LLD and the patient?s adult height will be less than if the shorter extremity had been lengthened. Correction of significant LLDs by this method may make a patient?s body look slightly disproportionate because of the shorter legs.
Causes
LLDs are very common. Sometimes the cause isn?t known. But the known causes of LLD in children include, injury or infection that slows growth of one leg bone. Injury to the growth plate (a soft part of a long bone that allows the bone to grow). Growth plate injury can slow bone growth in that leg. Fracture to a leg bone that causes overgrowth of the bone as it heals. A congenital (present at birth) problem (one whole side of the child?s body may be larger than the other side). Conditions that affect muscles and nerves, such as polio.
Symptoms
Children whose limbs vary in length often experience difficulty using their arms or legs. They might have difficulty walking or using both arms to engage in everyday activities.
Diagnosis
The evaluation of leg length discrepancy typically involves sequential x-rays to measure the exact discrepancy, while following its progression. In addition, an x-ray of the wrist allows us to more carefully age your child. Skeletal age and chronological age do not necessarily equal each other and frequently a child's bone age will be significantly different than his or her stated age. Your child's physician can establish a treatment plan once all the facts are known: the bone age, the exact amount of discrepancy, and the cause, if it can be identified.
Non Surgical Treatment
You may be prescribed a heel lift, which will equal out your leg length and decrease stress on your low back and legs. If it?s your pelvis causing the leg length discrepancy, then your physical therapist could use your muscles to realign your pelvis and then strengthen your core/abdominal region to minimize the risk of such malalignment happening again. If you think that one leg may be longer than the other and it is causing you to have pain or you are just curious, then make an appointment with a physical therapist.

can you stretch to get taller?
Surgical Treatment
Differences of an inch-and-a-half to two inches may require epiphysiodesis (adjusting the growth of the longer side) or acute shortening of the other side. Differences greater than 2.5 inches usually require a lengthening procedure. The short bone is cut and an external device is applied. Gradual lengthening is done over months to allow the muscles and nerves accommodate the new length.
Surgery is another option. In some cases the longer extremity can be shortened, but a major shortening may weaken the muscles of the extremity. In growing children, lower extremities can also be equalized by a surgical procedure that stops the growth at one or two sites of the longer extremity, while leaving the remaining growth undisturbed. Your physician can tell you how much equalization can be attained by surgically halting one or more growth centers. The procedure is performed under X-ray control through very small incisions in the knee area. This procedure will not cause an immediate correction in length. Instead, the LLD will gradually decrease as the opposite extremity continues to grow and "catch up." Timing of the procedure is critical; the goal is to attain equal length of the extremities at skeletal maturity, usually in the mid- to late teens. Disadvantages of this option include the possibility of slight over-correction or under-correction of the LLD and the patient?s adult height will be less than if the shorter extremity had been lengthened. Correction of significant LLDs by this method may make a patient?s body look slightly disproportionate because of the shorter legs.

Causes
LLDs are very common. Sometimes the cause isn?t known. But the known causes of LLD in children include, injury or infection that slows growth of one leg bone. Injury to the growth plate (a soft part of a long bone that allows the bone to grow). Growth plate injury can slow bone growth in that leg. Fracture to a leg bone that causes overgrowth of the bone as it heals. A congenital (present at birth) problem (one whole side of the child?s body may be larger than the other side). Conditions that affect muscles and nerves, such as polio.
Symptoms
Children whose limbs vary in length often experience difficulty using their arms or legs. They might have difficulty walking or using both arms to engage in everyday activities.
Diagnosis
The evaluation of leg length discrepancy typically involves sequential x-rays to measure the exact discrepancy, while following its progression. In addition, an x-ray of the wrist allows us to more carefully age your child. Skeletal age and chronological age do not necessarily equal each other and frequently a child's bone age will be significantly different than his or her stated age. Your child's physician can establish a treatment plan once all the facts are known: the bone age, the exact amount of discrepancy, and the cause, if it can be identified.
Non Surgical Treatment
You may be prescribed a heel lift, which will equal out your leg length and decrease stress on your low back and legs. If it?s your pelvis causing the leg length discrepancy, then your physical therapist could use your muscles to realign your pelvis and then strengthen your core/abdominal region to minimize the risk of such malalignment happening again. If you think that one leg may be longer than the other and it is causing you to have pain or you are just curious, then make an appointment with a physical therapist.

can you stretch to get taller?
Surgical Treatment
Differences of an inch-and-a-half to two inches may require epiphysiodesis (adjusting the growth of the longer side) or acute shortening of the other side. Differences greater than 2.5 inches usually require a lengthening procedure. The short bone is cut and an external device is applied. Gradual lengthening is done over months to allow the muscles and nerves accommodate the new length.
Leg Length Discrepancy Gait Study
Overview
You may be surprised to learn that most people have one leg that's just a bit longer than the other, or one foot that may be slightly larger. But for children with significant limb length discrepancies, the size difference between limbs can be a serious problem. There are two types of limb length discrepancies. Congenital discrepancy is when babies are born with one leg longer than the other. In some cases both legs are normal, except that one is shorter than the other. In other cases one particular part of the leg is underdeveloped or is absent. Acquired discrepancy is when babies are normal at birth, but some kind of injury happens, such as a severe fracture. The bone growth in that limb slows, which results in a leg length discrepancy that worsens as the child continues to grow.
Causes
There are many causes of leg length discrepancy. Some include, A broken leg bone may lead to a leg length discrepancy if it heals in a shortened position. This is more likely if the bone was broken in many pieces. It also is more likely if skin and muscle tissue around the bone were severely injured and exposed, as in an open fracture. Broken bones in children sometimes grow faster for several years after healing, causing the injured bone to become longer. A break in a child's bone through the growth center near the end of the bone may cause slower growth, resulting in a shorter leg. Bone infections that occur in children while they are growing may cause a significant leg length discrepancy. This is especially true if the infection happens in infancy. Inflammation of joints during growth may cause unequal leg length. One example is juvenile arthritis. Bone diseases may cause leg length discrepancy, as well. Examples are, Neurofibromatosis, Multiple hereditary exostoses, Ollier disease. Other causes include inflammation (arthritis) and neurologic conditions. Sometimes the cause of leg length discrepancy is unknown, particularly in cases involving underdevelopment of the inner or outer side of the leg, or partial overgrowth of one side of the body. These conditions are usually present at birth, but the leg length difference may be too small to be detected. As the child grows, the leg length discrepancy increases and becomes more noticeable. In underdevelopment, one of the two bones between the knee and the ankle is abnormally short. There also may be related foot or knee problems. Hemihypertrophy (one side too big) or hemiatrophy (one side too small) are rare leg length discrepancy conditions. In these conditions, the arm and leg on one side of the body are either longer or shorter than the arm and leg on the other side of the body. There may also be a difference between the two sides of the face. Sometimes no cause can be found. This is known as an "idiopathic" difference.
Symptoms
Often there are few or no symptoms prior to the age of 25-35. The most common symptom is chronic lower back pain, but also is frequently middle and upper back pain. Same-sided and repeated injury or pain to the hip, knee and/or ankle is also a hallmark of a long-standing untreated LLD. It is not uncommon to have buttock or radiating hip pain that is non-dermatomal (not from a disc) and tends to go away when lying down.
Diagnosis
Infants, children or adolescents suspected of having a limb-length condition should receive an evaluation at the first sign of difficulty in using their arms or legs. In many cases, signs are subtle and only noticeable in certain situations, such as when buying clothing or playing sports. Proper initial assessments by qualified pediatric orthopedic providers can reduce the likelihood of long-term complications and increase the likelihood that less invasive management will be effective. In most cases, very mild limb length discrepancies require no formal treatment at all.
Non Surgical Treatment
Internal heel lifts: Putting a simple heel lift inside the shoe or onto a foot orthotic has the advantage of being transferable to many pairs of shoes. It is also aesthetically more pleasing as the lift remains hidden from view. However, there is a limit as to how high the lift can be before affecting shoe fit. Dress shoes will usually only accommodate small lifts (1/8"1/4") before the heel starts to piston out of the shoe. Sneakers and workboots may allow higher lifts, e.g., up to 1/2", before heel slippage problems arise. External heel lifts: If a lift of greater than 1/2" is required, you should consider adding to the outsole of the shoe. In this way, the shoe fit remains good. Although some patients may worry about the cosmetics of the shoe, it does ensure better overall function. Nowadays with the development of synthetic foams and crepes, such lifts do not have to be as heavy as the cork buildups of the past. External buildups are not transferable and they will wear down over time, so the patient will need to be vigilant in having them repaired. On ladies' high-heel shoes, it may be possible to lower one heel and thereby correct the imbalance.

how to increase height after 21
Surgical Treatment
Surgical operations to equalize leg lengths include the following. Shortening the longer leg. This is usually done if growth is already complete, and the patient is tall enough that losing an inch is not a problem. Slowing or stopping the growth of the longer leg. Growth of the lower limbs take place mainly in the epiphyseal plates (growth plates) of the lower femur and upper tibia and fibula. Stapling the growth plates in a child for a few years theoretically will stop growth for the period, and when the staples were removed, growth was supposed to resume. This procedure was quite popular till it was found that the amount of growth retarded was not certain, and when the staples where removed, the bone failed to resume its growth. Hence epiphyseal stapling has now been abandoned for the more reliable Epiphyseodesis. By use of modern fluoroscopic equipment, the surgeon can visualize the growth plate, and by making small incisions and using multiple drillings, the growth plate of the lower femur and/or upper tibia and fibula can be ablated. Since growth is stopped permanently by this procedure, the timing of the operation is crucial. This is probably the most commonly done procedure for correcting leg length discrepancy. But there is one limitation. The maximum amount of discrepancy that can be corrected by Epiphyseodesis is 5 cm. Lengthening the short leg. Various procedures have been done over the years to effect this result. External fixation devices are usually needed to hold the bone that is being lengthened. In the past, the bone to be lengthened was cut, and using the external fixation device, the leg was stretched out gradually over weeks. A gap in the bone was thus created, and a second operation was needed to place a bone block in the gap for stability and induce healing as a graft. More recently, a new technique called callotasis is being use. The bone to be lengthened is not cut completely, only partially and called a corticotomy. The bone is then distracted over an external device (usually an Ilizarov or Orthofix apparatus) very slowly so that bone healing is proceeding as the lengthening is being done. This avoids the need for a second procedure to insert bone graft. The procedure involved in leg lengthening is complicated, and fraught with risks. Theoretically, there is no limit to how much lengthening one can obtain, although the more ambitious one is, the higher the complication rate.
You may be surprised to learn that most people have one leg that's just a bit longer than the other, or one foot that may be slightly larger. But for children with significant limb length discrepancies, the size difference between limbs can be a serious problem. There are two types of limb length discrepancies. Congenital discrepancy is when babies are born with one leg longer than the other. In some cases both legs are normal, except that one is shorter than the other. In other cases one particular part of the leg is underdeveloped or is absent. Acquired discrepancy is when babies are normal at birth, but some kind of injury happens, such as a severe fracture. The bone growth in that limb slows, which results in a leg length discrepancy that worsens as the child continues to grow.

Causes
There are many causes of leg length discrepancy. Some include, A broken leg bone may lead to a leg length discrepancy if it heals in a shortened position. This is more likely if the bone was broken in many pieces. It also is more likely if skin and muscle tissue around the bone were severely injured and exposed, as in an open fracture. Broken bones in children sometimes grow faster for several years after healing, causing the injured bone to become longer. A break in a child's bone through the growth center near the end of the bone may cause slower growth, resulting in a shorter leg. Bone infections that occur in children while they are growing may cause a significant leg length discrepancy. This is especially true if the infection happens in infancy. Inflammation of joints during growth may cause unequal leg length. One example is juvenile arthritis. Bone diseases may cause leg length discrepancy, as well. Examples are, Neurofibromatosis, Multiple hereditary exostoses, Ollier disease. Other causes include inflammation (arthritis) and neurologic conditions. Sometimes the cause of leg length discrepancy is unknown, particularly in cases involving underdevelopment of the inner or outer side of the leg, or partial overgrowth of one side of the body. These conditions are usually present at birth, but the leg length difference may be too small to be detected. As the child grows, the leg length discrepancy increases and becomes more noticeable. In underdevelopment, one of the two bones between the knee and the ankle is abnormally short. There also may be related foot or knee problems. Hemihypertrophy (one side too big) or hemiatrophy (one side too small) are rare leg length discrepancy conditions. In these conditions, the arm and leg on one side of the body are either longer or shorter than the arm and leg on the other side of the body. There may also be a difference between the two sides of the face. Sometimes no cause can be found. This is known as an "idiopathic" difference.
Symptoms
Often there are few or no symptoms prior to the age of 25-35. The most common symptom is chronic lower back pain, but also is frequently middle and upper back pain. Same-sided and repeated injury or pain to the hip, knee and/or ankle is also a hallmark of a long-standing untreated LLD. It is not uncommon to have buttock or radiating hip pain that is non-dermatomal (not from a disc) and tends to go away when lying down.
Diagnosis
Infants, children or adolescents suspected of having a limb-length condition should receive an evaluation at the first sign of difficulty in using their arms or legs. In many cases, signs are subtle and only noticeable in certain situations, such as when buying clothing or playing sports. Proper initial assessments by qualified pediatric orthopedic providers can reduce the likelihood of long-term complications and increase the likelihood that less invasive management will be effective. In most cases, very mild limb length discrepancies require no formal treatment at all.
Non Surgical Treatment
Internal heel lifts: Putting a simple heel lift inside the shoe or onto a foot orthotic has the advantage of being transferable to many pairs of shoes. It is also aesthetically more pleasing as the lift remains hidden from view. However, there is a limit as to how high the lift can be before affecting shoe fit. Dress shoes will usually only accommodate small lifts (1/8"1/4") before the heel starts to piston out of the shoe. Sneakers and workboots may allow higher lifts, e.g., up to 1/2", before heel slippage problems arise. External heel lifts: If a lift of greater than 1/2" is required, you should consider adding to the outsole of the shoe. In this way, the shoe fit remains good. Although some patients may worry about the cosmetics of the shoe, it does ensure better overall function. Nowadays with the development of synthetic foams and crepes, such lifts do not have to be as heavy as the cork buildups of the past. External buildups are not transferable and they will wear down over time, so the patient will need to be vigilant in having them repaired. On ladies' high-heel shoes, it may be possible to lower one heel and thereby correct the imbalance.

how to increase height after 21
Surgical Treatment
Surgical operations to equalize leg lengths include the following. Shortening the longer leg. This is usually done if growth is already complete, and the patient is tall enough that losing an inch is not a problem. Slowing or stopping the growth of the longer leg. Growth of the lower limbs take place mainly in the epiphyseal plates (growth plates) of the lower femur and upper tibia and fibula. Stapling the growth plates in a child for a few years theoretically will stop growth for the period, and when the staples were removed, growth was supposed to resume. This procedure was quite popular till it was found that the amount of growth retarded was not certain, and when the staples where removed, the bone failed to resume its growth. Hence epiphyseal stapling has now been abandoned for the more reliable Epiphyseodesis. By use of modern fluoroscopic equipment, the surgeon can visualize the growth plate, and by making small incisions and using multiple drillings, the growth plate of the lower femur and/or upper tibia and fibula can be ablated. Since growth is stopped permanently by this procedure, the timing of the operation is crucial. This is probably the most commonly done procedure for correcting leg length discrepancy. But there is one limitation. The maximum amount of discrepancy that can be corrected by Epiphyseodesis is 5 cm. Lengthening the short leg. Various procedures have been done over the years to effect this result. External fixation devices are usually needed to hold the bone that is being lengthened. In the past, the bone to be lengthened was cut, and using the external fixation device, the leg was stretched out gradually over weeks. A gap in the bone was thus created, and a second operation was needed to place a bone block in the gap for stability and induce healing as a graft. More recently, a new technique called callotasis is being use. The bone to be lengthened is not cut completely, only partially and called a corticotomy. The bone is then distracted over an external device (usually an Ilizarov or Orthofix apparatus) very slowly so that bone healing is proceeding as the lengthening is being done. This avoids the need for a second procedure to insert bone graft. The procedure involved in leg lengthening is complicated, and fraught with risks. Theoretically, there is no limit to how much lengthening one can obtain, although the more ambitious one is, the higher the complication rate.
Mortons Neuroma Treatment
Overview
 A Morton's neuroma is a benign (noncancerous) swelling along a nerve in the foot that carries sensations from the toes. The reason the nerve starts to swell is unknown. But once swelling begins, the nearby bones and ligaments put pressure on the nerve, causing more irritation and inflammation. This produces burning pain, numbness, tingling and other abnormal sensations in the toes. A Morton's neuroma also is called an interdigital neuroma, intermetatarsal neuroma or a forefoot neuroma.
A Morton's neuroma is a benign (noncancerous) swelling along a nerve in the foot that carries sensations from the toes. The reason the nerve starts to swell is unknown. But once swelling begins, the nearby bones and ligaments put pressure on the nerve, causing more irritation and inflammation. This produces burning pain, numbness, tingling and other abnormal sensations in the toes. A Morton's neuroma also is called an interdigital neuroma, intermetatarsal neuroma or a forefoot neuroma.
Causes
Morton's Neuroma is a foot condition caused from an abnormal function of the foot that leads to bones squeezing a nerve usually between the 3rd and 4th metatarsal heads. Symptoms of Morton's Neuroma often occur during or after you have been placing significant pressure on the forefoot area, while walking, standing, jumping, or sprinting. This condition can also be caused by footwear selection. Footwear with pointed toes and/or high heels can often lead to a neuroma. Constricting shoes can pinch the nerve between the toes, causing discomfort and extreme pain.
Symptoms
Symptoms of interdigital neuroma typically manifest as a sharp, burning or tingling sensation in the forefoot. The pain radiates toward the lesser toes and is aggravated by shoe wear. The pain is relieved when the shoe is removed and the forefoot is massaged. Sometimes the symptoms involve specific toes.
Diagnosis
The clinical symptoms should quickly lead your doctor to suspect a neuroma. When examined, the doctor may feel a "click" which is known as Mulder's sign. There may be tenderness in the interspace. The metatarsal bones will also be examined both clinically (and often with an xray). Tenderness at one of the metatarsal bones can suggest an overstress reaction (pre-stress fracture or stress fracture) in the bone. An ultrasound scan can confirm the diagnosis and is a less expensive and at this time, at least as sensitive a test as an MRI. An x-ray does not show neuromas, but can be useful to "rule out" other causes of the pain.
Non Surgical Treatment
If your Morton's neuroma is painful, your doctor usually will begin treatment with conservative therapies, including a switch to shoes with low heels, wide toes and good arch support. Padding techniques, including metatarsal pads or toe crest pads. Shoe inserts (orthotics) to help correct any mechanical imbalance in the foot. Anti-inflammatory medication, such as ibuprofen (Advil, Motrin and other brand names) or naproxen (Aleve, Naprosyn and other brand names) A local injection of anesthetic and corticosteroid medication into the affected area. Inflamed or injured nerves can take months to improve, even after the underlying problem has been corrected.
Surgical Treatment
Surgery to remove the neuroma may be recommended if more conservative treatment does not solve the problem. While surgery usually relieves or completely removes the symptoms, it often leaves a permanent numb feeling at the site of the neuroma.
Prevention
To help reduce your chance of developing Morton's neuroma avoid wearing tight and/or high-heeled shoes. Maintain or achieve ideal body weight. If you play sports, wear roomy, properly fitting athletic footwear.
 A Morton's neuroma is a benign (noncancerous) swelling along a nerve in the foot that carries sensations from the toes. The reason the nerve starts to swell is unknown. But once swelling begins, the nearby bones and ligaments put pressure on the nerve, causing more irritation and inflammation. This produces burning pain, numbness, tingling and other abnormal sensations in the toes. A Morton's neuroma also is called an interdigital neuroma, intermetatarsal neuroma or a forefoot neuroma.
A Morton's neuroma is a benign (noncancerous) swelling along a nerve in the foot that carries sensations from the toes. The reason the nerve starts to swell is unknown. But once swelling begins, the nearby bones and ligaments put pressure on the nerve, causing more irritation and inflammation. This produces burning pain, numbness, tingling and other abnormal sensations in the toes. A Morton's neuroma also is called an interdigital neuroma, intermetatarsal neuroma or a forefoot neuroma.Causes
Morton's Neuroma is a foot condition caused from an abnormal function of the foot that leads to bones squeezing a nerve usually between the 3rd and 4th metatarsal heads. Symptoms of Morton's Neuroma often occur during or after you have been placing significant pressure on the forefoot area, while walking, standing, jumping, or sprinting. This condition can also be caused by footwear selection. Footwear with pointed toes and/or high heels can often lead to a neuroma. Constricting shoes can pinch the nerve between the toes, causing discomfort and extreme pain.
Symptoms
Symptoms of interdigital neuroma typically manifest as a sharp, burning or tingling sensation in the forefoot. The pain radiates toward the lesser toes and is aggravated by shoe wear. The pain is relieved when the shoe is removed and the forefoot is massaged. Sometimes the symptoms involve specific toes.
Diagnosis
The clinical symptoms should quickly lead your doctor to suspect a neuroma. When examined, the doctor may feel a "click" which is known as Mulder's sign. There may be tenderness in the interspace. The metatarsal bones will also be examined both clinically (and often with an xray). Tenderness at one of the metatarsal bones can suggest an overstress reaction (pre-stress fracture or stress fracture) in the bone. An ultrasound scan can confirm the diagnosis and is a less expensive and at this time, at least as sensitive a test as an MRI. An x-ray does not show neuromas, but can be useful to "rule out" other causes of the pain.
Non Surgical Treatment
If your Morton's neuroma is painful, your doctor usually will begin treatment with conservative therapies, including a switch to shoes with low heels, wide toes and good arch support. Padding techniques, including metatarsal pads or toe crest pads. Shoe inserts (orthotics) to help correct any mechanical imbalance in the foot. Anti-inflammatory medication, such as ibuprofen (Advil, Motrin and other brand names) or naproxen (Aleve, Naprosyn and other brand names) A local injection of anesthetic and corticosteroid medication into the affected area. Inflamed or injured nerves can take months to improve, even after the underlying problem has been corrected.

Surgical Treatment
Surgery to remove the neuroma may be recommended if more conservative treatment does not solve the problem. While surgery usually relieves or completely removes the symptoms, it often leaves a permanent numb feeling at the site of the neuroma.
Prevention
To help reduce your chance of developing Morton's neuroma avoid wearing tight and/or high-heeled shoes. Maintain or achieve ideal body weight. If you play sports, wear roomy, properly fitting athletic footwear.
Shoe Lifts The Solution To Leg Length Discrepancy
There are actually two unique variations of leg length discrepancies, congenital and acquired. Congenital implies that you are born with it. One leg is structurally shorter than the other. Through developmental phases of aging, the human brain senses the stride pattern and recognizes some variance. The body typically adapts by dipping one shoulder over to the "short" side. A difference of under a quarter inch is not really excessive, doesn't need Shoe Lifts to compensate and normally doesn't have a serious effect over a lifetime.

Leg length inequality goes typically undiagnosed on a daily basis, however this condition is very easily fixed, and can reduce many cases of lumbar pain.
Therapy for leg length inequality typically involves Shoe Lifts. Many are very reasonably priced, typically costing below twenty dollars, in comparison to a custom orthotic of $200 or higher. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position.
Lumbar pain is the most common health problem impacting people today. Over 80 million people experience back pain at some stage in their life. It's a problem which costs companies huge amounts of money annually because of lost time and production. Fresh and improved treatment methods are constantly sought after in the hope of minimizing the economic influence this issue causes.

Men and women from all corners of the world experience foot ache as a result of leg length discrepancy. In these types of situations Shoe Lifts are usually of very useful. The lifts are capable of easing any pain in the feet. Shoe Lifts are recommended by many skilled orthopaedic orthopedists.
So that they can support the body in a balanced manner, your feet have a critical function to play. Despite that, it can be the most overlooked region in the body. Many people have flat-feet meaning there is unequal force exerted on the feet. This causes other areas of the body like knees, ankles and backs to be affected too. Shoe Lifts guarantee that the right posture and balance are restored.

Leg length inequality goes typically undiagnosed on a daily basis, however this condition is very easily fixed, and can reduce many cases of lumbar pain.
Therapy for leg length inequality typically involves Shoe Lifts. Many are very reasonably priced, typically costing below twenty dollars, in comparison to a custom orthotic of $200 or higher. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position.
Lumbar pain is the most common health problem impacting people today. Over 80 million people experience back pain at some stage in their life. It's a problem which costs companies huge amounts of money annually because of lost time and production. Fresh and improved treatment methods are constantly sought after in the hope of minimizing the economic influence this issue causes.

Men and women from all corners of the world experience foot ache as a result of leg length discrepancy. In these types of situations Shoe Lifts are usually of very useful. The lifts are capable of easing any pain in the feet. Shoe Lifts are recommended by many skilled orthopaedic orthopedists.
So that they can support the body in a balanced manner, your feet have a critical function to play. Despite that, it can be the most overlooked region in the body. Many people have flat-feet meaning there is unequal force exerted on the feet. This causes other areas of the body like knees, ankles and backs to be affected too. Shoe Lifts guarantee that the right posture and balance are restored.
The Causes Of Calcaneal Spur
Overview
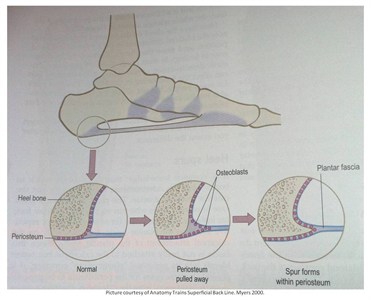
A heel spur (or osteophyte) is a small bony growth or collection of bony growths on the back or underside of the heel. They may or may not cause pain, and patients often confuse heel spurs with a related condition known as plantar fasciitis, inflammation of the band of tissue that stretches from the ball of the foot to the heel, forming the arch. Many people have bone spurs without ever knowing it, and about 70 percent of patients with plantar fasciitis who do have discomfort will also be found to have a heel spur when observed via X-ray. It is likely that a bone spur forms as the body tries to repair itself from repeated injury by laying down extra bone at the site of trauma. Plantar fasciitis is typically another result of such trauma. Heel spurs are most often seen in middle-aged men and women, but can be found in all age groups.
Causes
A strong band of sinew (plantar fascia) stretches across the sole of the foot below the surface of the skin and is attached to a point in the middle of the under surface of the heel bone. With repeated activity on our feet, the plantar fascia can become tight and cause persistent traction (tugging) on its attachment point into the heel bone, and inflammation and pain may develop at this site. This painful condition is known as plantar fasciitis. Sometimes a ?spur? develops at the site of this traction on the bone and protrudes into the surrounding tissue. This is a heel spur.
.gif)
Symptoms
Most heel spurs cause no symptoms and may go undetected for years. If they cause no pain or discomfort, they require no treatment. Occasionally, a bone spur will break off from the larger bone, becoming a ?loose body?, floating in a joint or embedding itself in the lining of the joint. This can cause pain and intermittent locking of the joint. In the case of heel spurs, sharp pain and discomfort is felt on the bottom of the foot or heel.
Diagnosis
Your doctor, when diagnosing and treating this condition will need an x-ray and sometimes a gait analysis to ascertain the exact cause of this condition. If you have pain in the bottom of your foot and you do not have diabetes or a vascular problem, some of the over-the-counter anti-inflammatory products such as Advil or Ibuprofin are helpful in eradicating the pain. Pain creams, such as Neuro-eze, BioFreeze & Boswella Cream can help to relieve pain and help increase circulation.
Non Surgical Treatment
Common and effective treatments for Heel Spurs include: Stretching exercises, changing to specific shoes, taping or strapping to rest stressed muscles and tendons, custom orthotic devices and physiotherapy. There are many things you can do to treat heel spurs. You should stretch the muscles and ligaments around the area regularly and ensure you are wearing the right footwear for your feet. There are also tapes and straps that you can apply to the muscles and tendons around the area. For more severe cases, custom orthotics may be the way to go along with aggressive physiotherapy. To treat the pain, over the counter NSAIDs (anti-inflammatory medications) is recommended, but use with caution as prolonged use can lead to the development of ulcers. It is therefore best to apply a topical treatment such as Zax?s Original Heelspur Cream, which contains natural ingredients proven to reduce pain and inflammation. More severe forms of the condition may require corticosteroid injections or surgical procedures, but these are very rare cases. Still, should pain become worse and persist, you should consult with your doctor.
Surgical Treatment
Most studies indicate that 95% of those afflicted with heel spurs are able to relieve their heel pain with nonsurgical treatments. If you are one of the few people whose symptoms don?t improve with other treatments, your doctor may recommend plantar fascia release surgery. Plantar fascia release involves cutting part of the plantar fascia ligament in order to release the tension and relieve the inflammation of the ligament. Sometimes the bone spur is also removed, if there is a large spur (remember that the bone spur is rarely a cause of pain. Overall, the success rate of surgical release is 70 to 90 percent in patients with heel spurs. One should always be sure to understand all the risks associated with any surgery they are considering.